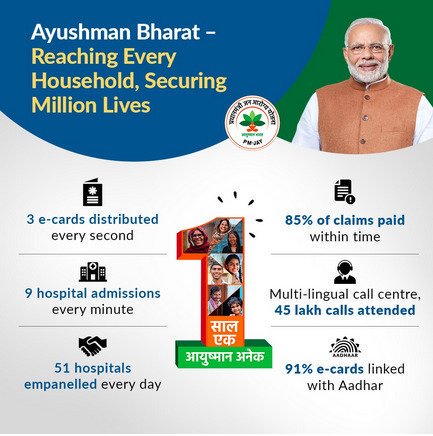
NEW DELHI: There were nine hospital admissions every minute across India in the first year of the government’s flagship Ayushman Bharat health insurance scheme, which has crossed the 50 lakh treatment mark.
According to official data, free secondary and tertiary treatment worth Rs 7,901 crore has been carried out in the 32 states and Union territories already implementing the Pradhan Mantri Jan Arogya Yojna (PMJAY) till October 14.
More than 60 per cent of the amount spent has been on tertiary care. Cardiology, orthopaedics, radiation oncology, cardio-thoracic and vascular surgery and urology emerged as the top tertiary specialities.
Lauding the progress of the scheme, Union Health Minister Harsh Vardhan said, “The Ayushman Bharat family is growing by leaps and bounds. In just over one year, under PM-JAY more than 50 lakh treatments have been availed by beneficiaries across the country. The successful implementation of this scheme will help us take forward Pandit Deen Dayal Upadhyay’s vision of ‘Antyodaya’ the uplift of the last man.”
“The scheme will continue to focus on reducing catastrophic out-of-pocket health expenditure, improving access to quality health care and meeting the unmet need of the population for hospitalization care, so that we move towards the vision of universal health coverage,” Dr Indu Bhushan, CEO, NHA, the apex body responsible for implementing the scheme, said.
The 50 lakh hospital admissions have taken place in the public and empanelled private hospitals that provide care to the beneficiaries under the scheme. Till date, 18,486 hospitals have been empanelled across India.
In the first year, 53 per cent of the empanelled hospitals are private, especially multi-specialty hospital. More than 50,000 people have availed treatment under the scheme outside their home states. The scheme gives annual healthcare benefits of up to Rs 5 lakh for every entitled family, and provides cashless and paperless access to services for the beneficiary at the point of service.
The National Health Authority (NHA) recently overhauled the existing health benefits packages of the AB-PMJAY, which includes revising their costs to remove any aberrations and discontinuation of around 554 packages.
Rates of 270 packages, including bypass surgery, temporary pacemaker implantation, knee replacement, breast cancer treatment, stone removal from kidney among others have been increased while prices of around 60 packages, including dialysis and cataract surgeries, have been reduced, an official said.
There is no change in the rates of 469 packages. Besides, there has been an introduction of 237 new packages and adoption of 43 stratified packages. PTI